✅ Abstract
Pediatric dental emergencies are critical situations requiring prompt diagnosis, calm communication, and effective intervention to relieve pain, prevent complications, and protect developing teeth.
📌 Recommended Article :
Dental Article 🔽 Management of acute orofacial infection of odontogenic origin in children - Diagnosis, clinic and pharmacology ... Infections of odontogenic origin are those that are generated and evolve from a tooth, either by a process of pulpal or periodontal infection. These infections spread to other tissues and put the patient's life at risk.This article reviews the most common emergencies, including trauma, infections, and soft tissue injuries, offering an evidence-based guide for clinical management.
Advertisement
✅ Introduction
In pediatric dentistry, emergencies are among the most stressful encounters for both practitioners and parents. Children often present with fear, pain, and anxiety, making communication and behavior management essential. The primary goals in these cases are alleviating pain, controlling infection, and preserving tooth structure and function. Proper training and a structured protocol allow clinicians to act efficiently while reassuring parents.
📌 Recommended Article :
Dental Article 🔽 Guidelines for the management of traumatic dental injuries in the primary dentition ... The lesions can compromise dental tissue (enamel, dentin, root), dental pulp, alveolar bone, and periodontal ligaments. Soft tissues such as lips and cheeks are also included.✅ Development
1. Classification of Pediatric Dental Emergencies
Emergencies can be classified into:
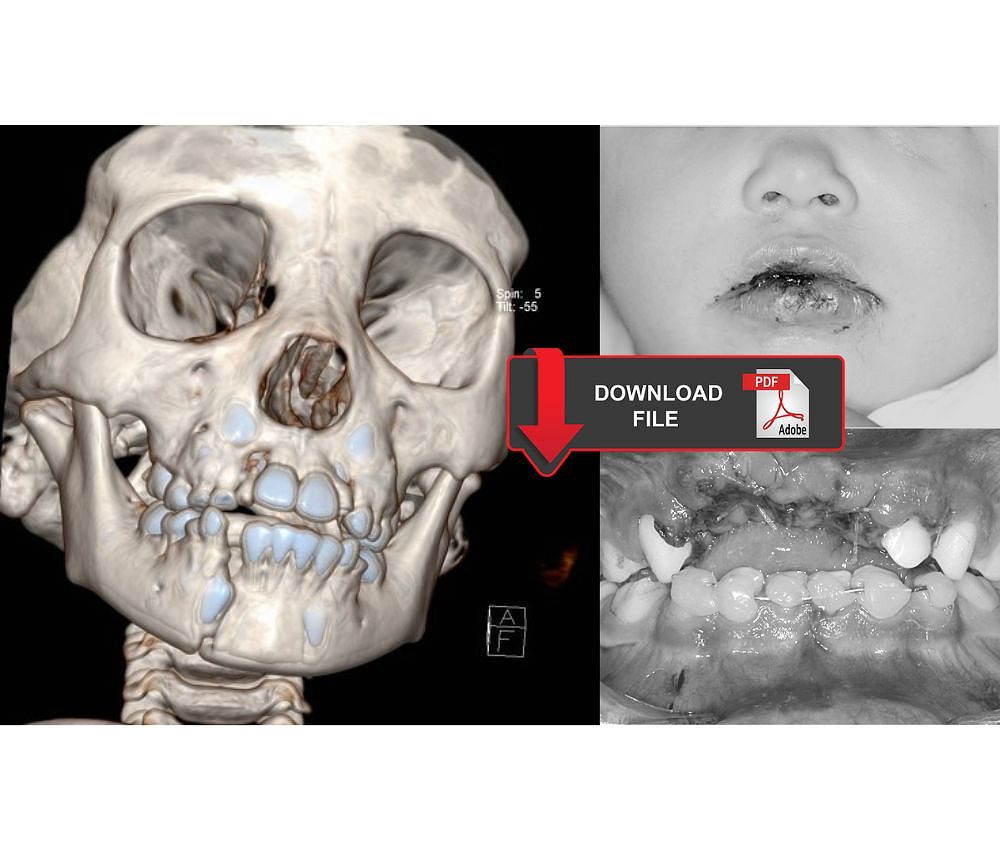
▪️ Traumatic dental injuries (fractures, luxations, avulsions)
▪️ Acute infections (pulpitis, abscesses, cellulitis)
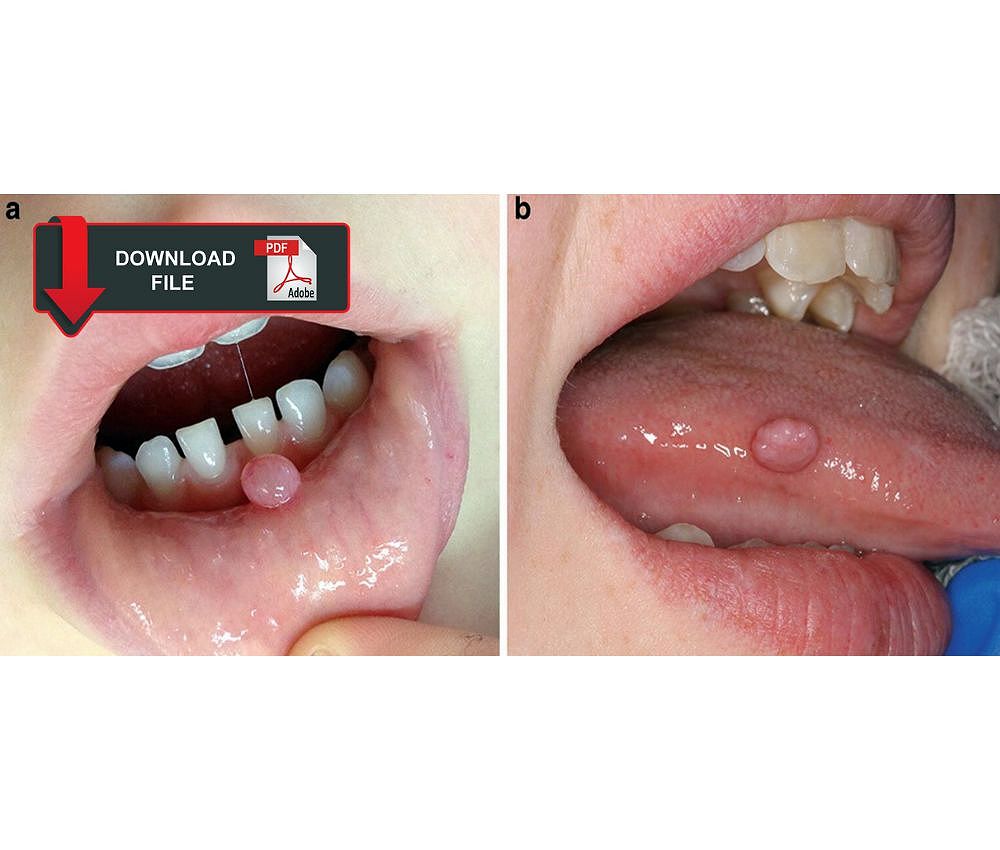
▪️ Soft tissue injuries (lacerations, hematomas)
▪️ Postoperative complications (pain, bleeding, or swelling)
Understanding these categories allows the clinician to prioritize care and implement an appropriate treatment sequence.
2. Initial Clinical Approach
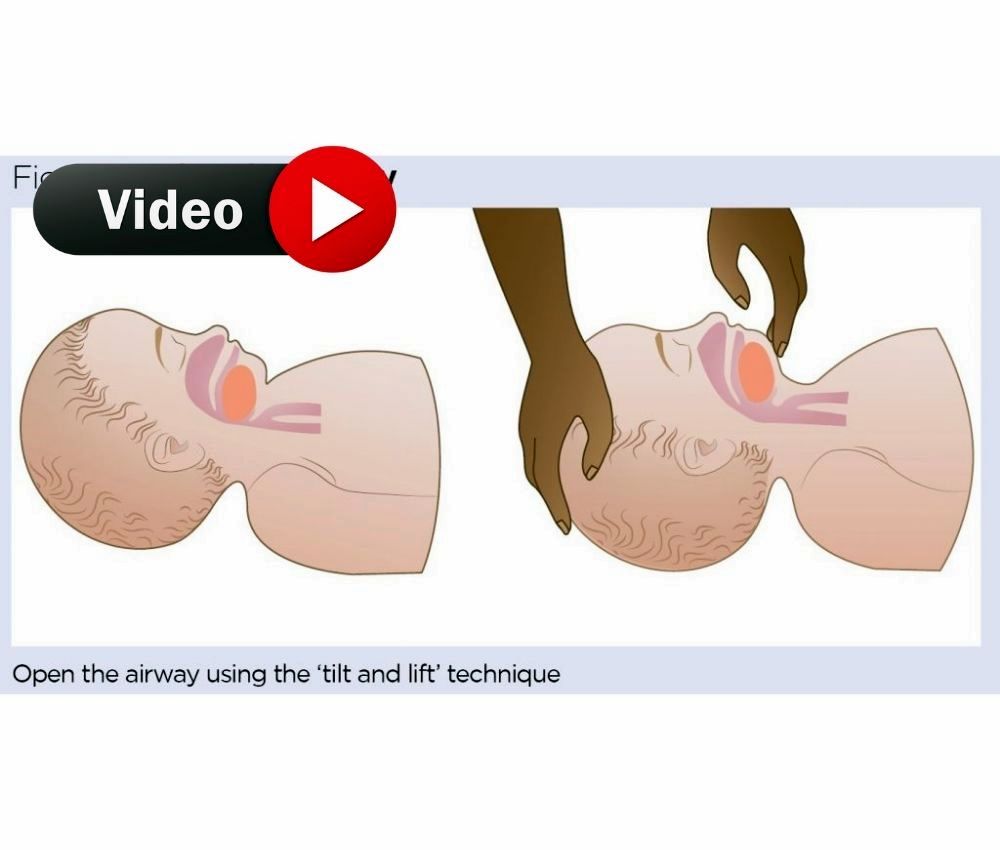
A systematic approach is key:
1. Calm the child and caregiver to reduce emotional stress.
2. Take a brief medical history, including allergies and previous reactions to medications.
3. Perform a quick extraoral and intraoral assessment to identify trauma, bleeding, or infection.
4. Apply immediate measures, such as hemostasis, cold compresses, or analgesics.
5. Plan definitive treatment, or refer to a specialist if necessary.
3. Management of Common Pediatric Dental Emergencies
Below is a comparative table summarizing the most frequent pediatric dental emergencies, their advantages of early management, and limitations if treatment is delayed.
📊 Comparative Table: Common Pediatric Dental Emergencies and Their Management
| Emergency Type | Early Management Benefits | Consequences of Delayed Care |
|---|---|---|
| Dental Trauma (fracture, avulsion) | Preserves tooth vitality; reduces risk of infection and resorption | Loss of tooth, ankylosis, or root resorption |
| Acute Pulpal or Periapical Infection | Rapid pain control and prevention of systemic spread | Cellulitis, fever, and possible airway compromise |
| Soft Tissue Injury | Promotes healing and prevents scarring | Infection or poor esthetic outcome |
| Postoperative Complications | Maintains child comfort and parental trust | Prolonged pain, bleeding, or loss of cooperation |
Pediatric dental emergencies require both technical skill and emotional intelligence. The practitioner must act swiftly while maintaining a child-centered approach. Evidence shows that early management of trauma and infection significantly improves outcomes (Andreasen et al., 2022). Moreover, parental education is fundamental—teaching them to store an avulsed tooth in milk, recognize infection signs, and seek immediate dental care can prevent severe complications.
📌 Recommended Article :
PDF 🔽 Reimplantation of avulsed permanent teeth after three days: Clinical case in a pediatric patient ... Dental avulsion consists of the total detachment of the tooth from the socket, as a consequence of a strong trauma that affects the oral cavity. Given this urgency, it is important to go to the dentist to be able to reimplant it.✍️ Conclusion
Pediatric dental emergencies demand preparedness, empathy, and clear communication. A calm approach, combined with structured clinical decision-making, ensures optimal outcomes. Establishing emergency protocols and educating parents can reduce anxiety and improve long-term oral health.
🔎 Recommendations
▪️ Keep an emergency kit with topical anesthetics, hemostatic agents, and splinting materials.
▪️ Train the dental team in pediatric behavior management and first aid.
▪️ Provide parents with educational materials on common emergencies and when to seek help.
▪️ Collaborate with pediatricians and emergency physicians for systemic cases.
📚 References
✔ Andreasen, J. O., Andreasen, F. M., & Lauridsen, E. (2022). Textbook and Color Atlas of Traumatic Injuries to the Teeth (6th ed.). Wiley-Blackwell.
✔ American Academy of Pediatric Dentistry (AAPD). (2023). Best Practices: Management of Acute Dental Trauma. https://www.aapd.org/research/oral-health-policies--recommendations/
✔ Malhotra, N., Kundabala, M., & Acharaya, S. (2021). Dental emergencies in children: Clinical management guidelines. Journal of Clinical Pediatric Dentistry, 45(2), 85–93. https://doi.org/10.17796/1053-4628-45.2.3
📌 More Recommended Items
► Reimplantation of avulsed dry permanent teeth after three days: A report of two cases
► What Are the Most Common Dental Emergencies and How Can You Manage Them?
► Webinar: Pediatric Dental Trauma and Odontogenic Infections - Dr. Kelly A. Kirtland DDS