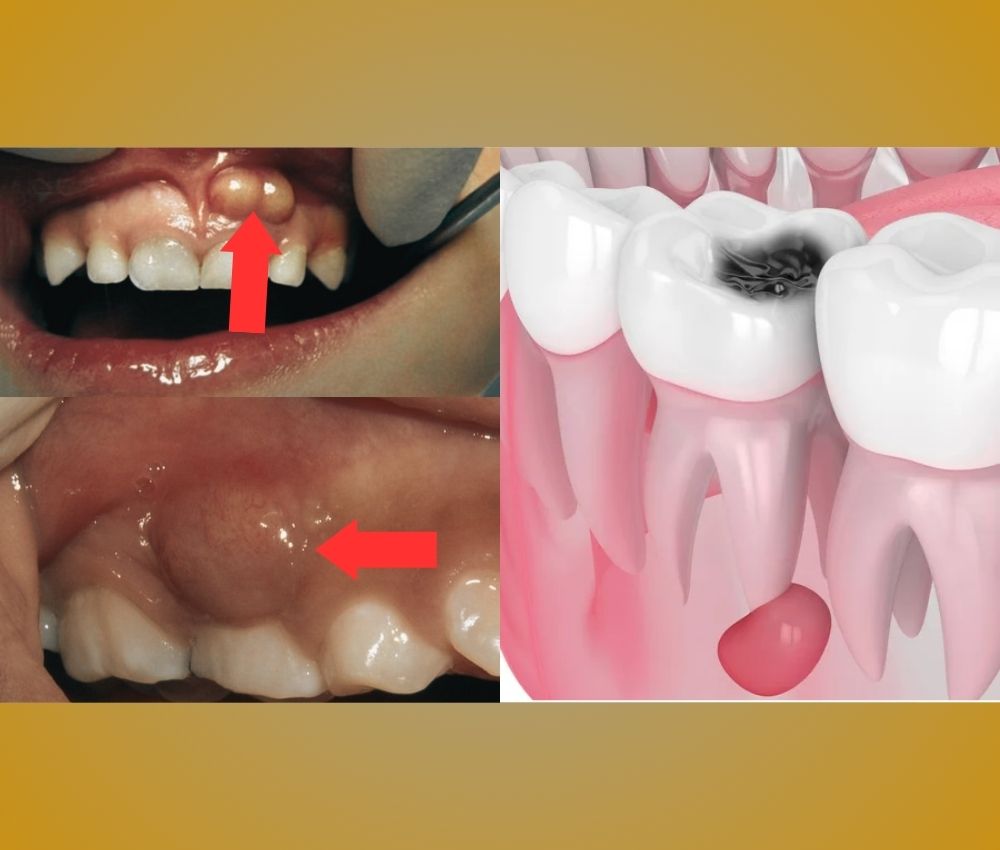
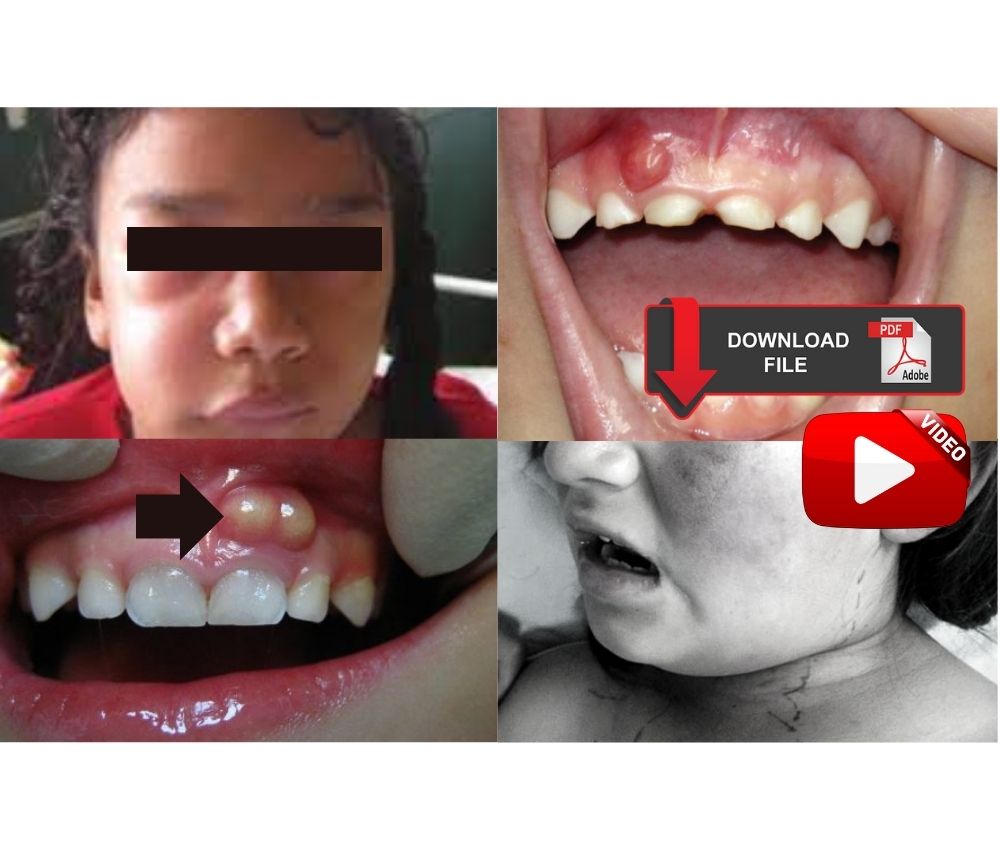
Odontogenic facial cellulitis in children is a diffuse, rapidly spreading bacterial infection of facial soft tissues originating from a dental source, most commonly untreated caries or pulp necrosis in primary teeth.
📌 Recommended Article :
Dental Article 🔽 How does hypertension affect oral health? ... Although our understanding of the pathophysiology of elevated arterial pressure has increased, in 90 to 95% of cases the etiology is still largely unknown.Unlike localized abscesses, cellulitis lacks a well-defined purulent collection and can progress quickly if not treated promptly.
Advertisement
✅ Clinical Evolution: From Mild to Severe Forms
➤ Early (Mild) Stage
▪️ Localized facial swelling
▪️ Mild erythema and warmth
▪️ Tenderness on palpation
▪️ Usually associated with a necrotic primary tooth
At this stage, systemic signs are often absent, and early intervention can prevent progression.
➤ Moderate Stage
▪️ Diffuse facial swelling with induration
▪️ Increased pain and discomfort
▪️ Low-grade fever
▪️ Regional lymphadenopathy
The infection begins to spread through facial planes, increasing the risk of complications.
➤ Severe Stage
▪️ Rapidly progressive facial edema
▪️ High fever and malaise
▪️ Trismus, dysphagia, or airway compromise
▪️ Periorbital or submandibular involvement
Severe odontogenic cellulitis in children is a medical emergency requiring immediate hospital-based management.
✅ Key Characteristics in Pediatric Patients
▪️ Faster progression due to immature immune response
▪️ Thinner cortical bone facilitating spread
▪️ Higher risk of dehydration and systemic involvement
▪️ Limited ability to verbalize symptoms clearly
📊 Comparative Table: Differences Between Pediatric and Adult Facial Cellulitis
| Aspect | Pediatric Patients | Adult Patients |
|---|---|---|
| Disease Progression | Rapid and aggressive spread through facial spaces | Generally slower and more localized progression |
| Immune Response | Immature immune system increases systemic risk | Mature immune response limits dissemination |
| Airway Compromise Risk | Higher risk due to anatomical and physiological factors | Lower risk in most cases |
| Bone and Tissue Anatomy | Thinner cortical bone facilitates infection spread | Denser bone offers greater resistance |
| Hospitalization Threshold | Lower threshold; early admission often required | Outpatient management more frequently possible |
➤ Initial Management
▪️ Prompt identification of the dental source
▪️ Assessment of airway, hydration, and systemic involvement
▪️ Early initiation of antibiotics
➤ Antibiotic Therapy
▪️ Mild cases: oral antibiotics (e.g., amoxicillin or amoxicillin–clavulanate)
▪️ Moderate to severe cases: intravenous antibiotics (e.g., ampicillin–sulbactam or clindamycin in penicillin-allergic patients)
➤ Definitive Dental Treatment
▪️ Extraction or pulp therapy of the involved tooth
▪️ Drainage if abscess formation occurs
Antibiotics alone are insufficient without elimination of the source of infection.
➤ Hospital Management
Indicated when:
▪️ Systemic symptoms are present
▪️ Facial spaces are involved
▪️ Oral intake is compromised
▪️ There is risk of airway obstruction
📊 Comparative Table: Differential Diagnosis of Pediatric Odontogenic Infections
| Aspect | Advantages | Limitations |
|---|---|---|
| Odontogenic Facial Cellulitis | Early detection allows rapid intervention | May progress quickly without clear abscess formation |
| Dental Abscess | Localized infection with defined drainage | May evolve into cellulitis if untreated |
| Lymphadenitis | Often self-limiting with supportive care | May mimic odontogenic infection clinically |
| Periorbital Cellulitis | Clear ophthalmologic signs aid diagnosis | High risk of serious complications |
The evolution of odontogenic facial cellulitis in children differs significantly from adults due to anatomical and immunological factors. Delayed diagnosis or inadequate management can result in severe complications, including deep neck infections and airway compromise. Current evidence supports early antibiotic therapy combined with definitive dental treatment.
🎯 Clinical Recommendations
▪️ Treat facial swelling of dental origin in children as potentially serious
▪️ Initiate antibiotics early but always remove the odontogenic focus
▪️ Refer for hospital care when systemic signs are present
▪️ Educate parents on early warning signs and urgency of treatment
✍️ Conclusion
Odontogenic facial cellulitis in pediatric patients is a rapidly evolving infection requiring prompt and aggressive management. Early recognition, appropriate antibiotic therapy, and elimination of the dental source are critical to preventing severe complications and ensuring favorable outcomes.
📚 References
✔ American Academy of Pediatric Dentistry. (2023). Management considerations for pediatric oral surgery and oral pathology. Pediatric Dentistry, 45(6), 412–420.
✔ Brook, I. (2017). Microbiology and management of odontogenic infections in children. Journal of Oral and Maxillofacial Surgery, 75(9), 1933–1941. https://doi.org/10.1016/j.joms.2017.03.023
✔ Rush, D. E., Abdel-Haq, N., Zhu, J. F., Aamar, B., & Malian, M. (2007). Childhood odontogenic infections: A review of 128 cases. Pediatric Dentistry, 29(6), 438–443.
✔ Flynn, T. R. (2011). Principles and surgical management of head and neck infections. Oral and Maxillofacial Surgery Clinics of North America, 23(3), 407–419. https://doi.org/10.1016/j.coms.2011.04.004
📌 More Recommended Items
► Wisdom Tooth Infection (Pericoronitis): Causes, Symptoms, and Evidence-Based Treatment
► When to Refer a Dental Infection to the Hospital: Indications and Severity Criteria
► Acute Versus Chronic Odontogenic Infections in Children: What the Pediatric Dentist Needs to Know